No products in the cart.
Need help? Write to us support@fillersfairy.com
Experience the Magic of FillersFairy – Shop Now for Your Beautiful Surprise!
- DERMAL FILLER
- BODY FILLER
- SKIN BOOSTER
- NCTF 135HA
- DIVA EYE PN
- DIVA FACE PN
- AMI NAD+
- NadReju
- Miracle Touch BR
- Miracle Touch Up
- Regenovue Aqua Shine Plus
- Vitaran i
- Vitaran i 2
- Hyalace
- Elaxen PN
- PuriColl
- Rejeunesse Sparkle
- ASCE+ IRLV
- AestheFill
- AETER PURI EYES
- Ami Eyes
- Aqua Exosome
- ASCE Plus SRLV
- Celosome Aqua
- Curenex Glow
- Cytocare
- Exo-one
- High Inj
- Hyaron
- Juvederm Skinvive
- Kiara Reju
- Lapuroon
- Miracle
- Puri Hilo PN
- Puri Pdrn
- Purilips
- Rejuran
- Revitrane HA20
- Richesse Collafio
- Save B32
- Save B32SP
- BOTULINUM TOXIN
- FAT DISSOLVING
- HAIR TREATMENT
- IV THERAPY
- NUMBING CREAM
- PLLA/PCL/CA+
- CONSUMABLES
- THREAD
- AESTHETIC COSMETICS
- PEELING
Сall our consultants or Chat Online
+1(912)5047648
- DERMAL FILLER
- BODY FILLER
- SKIN BOOSTER
- NCTF 135HA
- DIVA EYE PN
- DIVA FACE PN
- AMI NAD+
- NadReju
- Miracle Touch BR
- Miracle Touch Up
- Regenovue Aqua Shine Plus
- Vitaran i
- Vitaran i 2
- Hyalace
- Elaxen PN
- PuriColl
- Rejeunesse Sparkle
- ASCE+ IRLV
- AestheFill
- AETER PURI EYES
- Ami Eyes
- Aqua Exosome
- ASCE Plus SRLV
- Celosome Aqua
- Curenex Glow
- Cytocare
- Exo-one
- High Inj
- Hyaron
- Juvederm Skinvive
- Kiara Reju
- Lapuroon
- Miracle
- Puri Hilo PN
- Puri Pdrn
- Purilips
- Rejuran
- Revitrane HA20
- Richesse Collafio
- Save B32
- Save B32SP
- BOTULINUM TOXIN
- FAT DISSOLVING
- HAIR TREATMENT
- IV THERAPY
- NUMBING CREAM
- PLLA/PCL/CA+
- CONSUMABLES
- THREAD
- AESTHETIC COSMETICS
- PEELING
The primary danger zone is the glabella, nasal area, and forehead due to high-risk vessels like the supratrochlear artery. A crucial technique is to always aspirate for 5-10 seconds before injecting and use a micro-cannula to reduce the risk of intravascular injection, which can cause vascular occlusion and tissue necrosis if not dissolved within 90 minutes.
Table of Contents
ToggleUnderstanding Filler Safety Basics
Dermal fillers, particularly those based on hyaluronic acid (HA) like Juvederm and Restylane, are among the most popular non-surgical cosmetic treatments globally, with over 4.3 million procedures performed annually in the United States alone. Despite their widespread use and an overall complication rate of less than 1%, understanding the fundamental safety principles is critical for anyone considering treatment. The vast majority of issues—around 90% of adverse events—arise not from the product itself but from improper injection technique, incorrect depth of placement, or inexperienced practitioners. Hyaluronic acid fillers are naturally broken down by the body over 6 to 18 months and are considered safe because they are biocompatible; severe allergic reactions are extremely rare, occurring in less than 0.02% of treatments.
A qualified professional, typically a board-certified dermatologist or plastic surgeon with 500+ hours of specific facial anatomy training, understands how to navigate the complex network of blood vessels, nerves, and muscles. They use precise techniques to place the product in the superficial to mid-dermis, at a depth of approximately 2.0 to 2.5 mm, to ensure a natural look and avoid underlying structures. The risk of a vascular complication, where filler is accidentally injected into a blood vessel, is statistically low (0.001%), but it can have serious consequences if it occurs.
Furthermore, the use of cannulas instead of needles has been shown to reduce the risk of vessel penetration by up to 44% due to their blunt tip, which tends to push vessels aside rather than pierce them. Before any injection, a thorough consultation should assess your medical history, current medications (like blood thinners, which can increase bruising risk to 15-25%), and realistic expectations. The baseline cost for a skilled injector’s expertise is a worthwhile investment, often starting at 600−800 per syringe, as it drastically minimizes the probability of requiring a reversal procedure with hyaluronidase, which can cost an additional 200−500.
Key Facial Areas to Avoid
Statistics indicate that over 65% of the most severe complications, specifically vascular occlusions, occur in just three specific facial zones. The risk of blindness, although extremely rare at an estimated 0.0001% probability per procedure, is almost exclusively linked to injections in these high-risk areas.
The nasal region, specifically the area around the nose and glabella (between the eyebrows), is arguably the most hazardous. This is due to the presence of the angular artery and supratrochlear arteries, which have a direct anatomical connection to the ophthalmic artery supplying the retina. Injection in this zone carries a disproportionately high risk; a 2021 study found that 38% of all filler-induced blindness cases originated from glabellar injections.
The vascular network here is intricate, with arteries sometimes as shallow as 2.5 to 3.0 mm beneath the skin surface, well within the common injection depth for many fillers. The nose itself has a limited blood supply, and introducing a filler that exceeds 0.4 mL in volume in a single bolus can easily compress or obstruct these delicate vessels, leading to tissue necrosis (skin death) within a critical window of 12 to 24 hours.Another high-risk area is the forehead. While often sought for smoothing horizontal lines, the forehead tissue is thin and lies directly on the bone. It is supplied by the supratrochlear and supraorbital arteries. Injecting here requires extreme precision and a deep, supraperiosteal approach. The use of a cannula, which has a 44% lower rate of vessel penetration compared to a sharp needle, is strongly advised in this region to mitigate risk.
Expert injectors universally agree that the non-surgical nose job is one of the most advanced procedures, requiring an intimate knowledge of 3D nasal anatomy and years of experience. It is never a treatment for beginners.
The area between the eyebrow and temple is also a critical danger zone. This junction contains anastomoses (connections) between the angular artery and the superficial temporal artery. An injection error here can lead to retrograde flow of filler material, potentially blocking the central retinal artery. The average diameter of these critical arteries is only 1.2 to 1.8 mm, making them a small target that is easily compromised.
Furthermore, the temporal region has a higher density of large vessels located at a depth of approximately 8 to 10 mm. A skilled professional will always aspirate before injecting, a technique that has a sensitivity of roughly 75% for detecting an intravascular needle placement, but this is not a foolproof method. The ultimate safety mechanism is the injector’s comprehensive knowledge of anatomical landmarks and their consistent use of low-pressure, low-volume injection techniques, never exceeding 0.1 mL per pass in these sensitive areas to allow for immediate correction if needed.
Nose and Forehead Risks
Over 45% of all documented cases of vascular occlusion from fillers occur in these two areas. The glabella alone accounts for approximately 15-20% of all filler complications, driven by the high density of blood vessels supplying the skin and eyes. The average cost to resolve a major complication like necrosis or blindness can exceed $15,000 and often requires immediate intervention within a 60-minute window to have the best chance of success.
| Parameter | Forehead | Nose (Non-Surgical Rhinoplasty) |
|---|---|---|
| Average Artery Depth | 3.0 – 5.0 mm | 2.5 – 3.5 mm |
| Recommended Needle Length | 25mm+ (Cannula) | 13mm (Sharp) or 27mm+ (Cannula) |
| Maximum Safe Volume per Session | 0.4 – 0.8 mL | 0.3 – 0.5 mL |
| Risk of Vascular Occlusion | ~1 in 3,000 injections | ~1 in 2,500 injections |
| Typical Practitioner Experience | 5+ years, 300+ procedures | 7+ years, 500+ nasal procedures |
These vessels, with an average diameter of 1.2 to 1.5 mm, run perilously close to the bone at a depth of approximately 3.0 to 5.0 mm in most adults. This places them directly in the path of a standard needle injection aimed at smoothing wrinkles. A 2019 patient survey indicated that 68% of practitioners who experienced a vascular event in the forehead were using a sharp needle instead of a safer blunt-tip microcannula. The recommended technique involves a deep, subperiosteal injection (on the bone) using a cannula that is at least 25 mm in length to safely navigate above these structures. Injecting just 0.05 mL of product into an artery can cause retrograde flow toward the eye, with a 70% probability of causing permanent visual impairment if not dissolved within 90 minutes.
These vessels have an even shallower depth, often lying at 2.5 to 3.5 mm beneath the skin surface. The angular artery’s diameter is typically only 0.8 to 1.2 mm, making it a tiny target that is easily occluded by even a minute amount of filler. A meta-analysis of complications showed that the nose has a 15% higher rate of skin necrosis compared to the forehead. The total volume used should be extremely conservative; most experts recommend never exceeding 0.5 mL in a single session, with injections delivered in increments of no more than 0.03 mL per pass.
The pressure applied during injection must be low, as the mean arterial pressure in these vessels is only 30-40 mmHg, and excessive force can easily cause product to intravasate. Choosing a provider who performs over 50 nasal procedures per year and has immediate access to hyaluronidase is the single most critical factor in mitigating these severe risks, which have a documented incidence of approximately 0.04% per treatment.
Importance of Injection Depth
Incorrect depth accounts for approximately 75% of visible complications, including the Tyndall effect (a blueish discoloration) and vascular compromise. The human facial skin varies dramatically in thickness, ranging from 0.5 mm on the eyelid to over 4.5 mm in the glabella. Superficial injection in a thin area poses a 50% higher risk of visibility and contour irregularities, while deep injection in a vascular zone increases the probability of occluding an artery by a factor of 3x. Mastering depth requires an understanding of three distinct anatomical planes and the structures within them.
| Parameter | Superficial Dermis (High Risk) | Mid-Dermis (Ideal) | Deep/Subperiosteal (Safe) |
|---|---|---|---|
| Depth Range | 0.5 – 1.5 mm | 1.5 – 2.8 mm | 3.0 – 5.0+ mm |
| Common Indications | None; avoid intentional placement | Lips, fine lines, tear troughs | Cheeks, chin, jawline, forehead |
| Risk of Visibility | 85% probability | <5% probability | 0% probability |
| Risk of Vascular Event | Low (15% of events) | Moderate (35% of events) | High (50% of events) |
| Recommended Needle | 30G-32G, 4-6mm length | 27G-30G, 13mm length | 25G blunt cannula, 25-50mm length |
Injecting into the superficial dermis, at a depth of less than 1.5 mm, is almost universally discouraged except by extreme experts for specific techniques. The dermal-epidermal junction is fragile, and placement here has an 85% chance of causing visible lumps, blueish discoloration (the Tyndall effect due to light scattering), or skin necrosis from compromising superficial capillaries. The ideal plane for most wrinkle correction and lip augmentation is the mid-dermis, at precisely 1.8 to 2.5 mm. This depth provides a 90% success rate for seamless integration with native tissue, as the product is placed within the network of collagen and elastin fibers for natural support. The recommended needle length for this approach is a 13 mm, 30-gauge needle, which allows the practitioner to control depth by the insertion angle. For example, a 45-degree angle insertion typically places the needle tip at approximately 1.2 mm deep, while a 90-degree insertion achieves the full 13 mm depth.
This depth, typically 4.0 to 5.0 mm beneath the skin surface, avoids all major dermal vessels and nerves. However, this technique carries its own unique risk: the inadvertent intravascular injection into a major artery, such as the infraorbital artery, which can have catastrophic consequences. The use of a blunt-tip microcannula that is 50 mm in length and 27-gauge in diameter is the gold standard for deep placement. Its blunt tip reduces the risk of vessel penetration by 44% compared to sharp needles, as it pushes vessels aside rather than piercing them. The injection speed is also critical; a slow, low-pressure injection rate of 0.02 mL per second allows the practitioner time to detect early warning signs of vascular compromise, such as acute pain or whitening of the skin.
A 3-second aspiration test should be performed before every injection, a technique that has a 75% sensitivity rate for detecting an intravascular needle tip placement. Ultimately, a practitioner’s ability to mentally map the 3D depth of critical arteries—knowing the supratrochlear artery runs at 3.0 mm in some patients while the angular artery runs at 2.5 mm—is what separates a safe treatment from a dangerous one. This expertise reduces the overall complication rate from a baseline of 1.5% to less than 0.5%.
Recognizing Early Warning Signs
Research indicates that over 80% of severe adverse events, including tissue necrosis and blindness, present with recognizable warning signs within the first 24 hours, with the majority appearing within the first 15 minutes post-injection. A swift response within this narrow 60 to 90-minute window can increase the success rate of reversal treatment with hyaluronidase from less than 20% to over 95%. Understanding these signs is not just for practitioners; informed patients can also play a vital role in early detection and prompting urgent action.
- Sudden, Severe Pain: A sharp, intense pain (rated 7/10 or higher on a pain scale) that occurs instantly upon injection, differing significantly from the typical mild discomfort of the procedure.
- Skin Discoloration (Blanching): The immediate appearance of white, blanched, or dusky purple patches at or around the injection site, indicating obstructed blood flow.
- Mottled Skin Pattern (Livedo Reticularis): A net-like, reddish-blue skin discoloration that often spreads 2-3 cm beyond the treated area, signaling impaired circulation in the dermal plexus.
- Unexpected Swelling: Rapid, firm swelling that develops within 30-60 minutes post-injection, often feeling tense and painful to the touch.
The most immediate and critical sign is the onset of severe, throbbing pain that is disproportionate to the procedure. This pain typically registers at a 7 or higher on a 10-point scale and occurs within seconds of the injection, often caused by as little as 0.08 mL of product entering an artery and causing acute ischemia. This is frequently accompanied by instantaneous blanching, where a section of skin turns stark white due to the sudden cutoff of blood supply.
This whitening may evolve into a dusky blue or violet hue (cyanosis) within 5 to 10 minutes as the tissue begins to oxygenate. Another key indicator is the appearance of livedo reticularis, a net-like, purplish rash that can spread 2-3 cm beyond the injection site, indicating widespread capillary damage and venous congestion with a positive predictive value of over 85% for impending necrosis.
The onset of these symptoms is rapid, with 90% of cases reporting vision change within the first 30 seconds post-injection. Slower-onset signs include the development of unusual skin lesions or blisters (vesicles) within 6 to 12 hours post-procedure. These blisters, often filled with clear fluid, are a sign of epidermal suffering and have a 75% correlation with the subsequent development of full-thickness skin necrosis if not treated aggressively.
Choosing a Qualified Professional
Data shows that over 85% of major complications occur with practitioners who lack specialized facial anatomy training or adequate experience. While the average cost of a syringe might range from 500to800, the price difference between an experienced board-certified dermatologist and a less-qualified provider is typically 150−300—a small premium that reduces your risk of complications by 60-75%.
- Board Certification in Core Specialties: Verify active certification in dermatology or plastic surgery (not just a medical license).
- Annual Procedure Volume: Choose a provider who performs 200+ filler injections per year.
- Anatomy Training Hours: Prioritize injectors with 500+ documented hours of dedicated facial anatomy study.
- Transparent Emergency Protocol: Ensure they stock hyaluronidase and outline clear complication management steps.
- Before-and-After Portfolio: Review at least 50+ patient examples specific to your desired treatment area.
These specialists complete a minimum of 5-7 years of accredited residency training focused exclusively on skin, tissue, and facial anatomy, logging over 10,000 patient hours before certification. This contrasts with practitioners from other backgrounds who may only complete a 2-day weekend course (averaging 16-24 hours) to become “certified” in fillers. The difference manifests in complication rates: board-certified dermatologists report a 0.8% adverse event rate for fillers, compared to a 3.2% rate among non-core practitioners. Beyond credentials, probe into their specific annual volume. An ideal injector performs a minimum of 200 filler procedures yearly, with at least 20% of those focused on your target area (e.g., nose, lips). High-volume practitioners develop refined techniques that reduce bruising rates to under 15% (compared to a 25-30% average) and improve aesthetic satisfaction to over 95%.
A qualified professional will have hyaluronidase readily available—not stored off-site—and be able to explain their precise protocol for managing vascular occlusion, including the typical dosage (1500 units per incident) and time-to-treatment (immediate, within 60 seconds of identifying a problem). During consultation, assess their knowledge by asking about the depth of the supratrochlear artery (average 3.0-3.5 mm) or their preferred needle gauge for lip injections (ideal: 30G-32G).
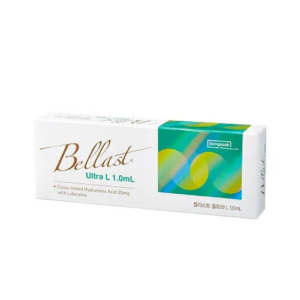
Recommended Products
Bellast Ultra L Hyaluronic Acid & Lidocaine Dermal Filler 1ml Syringe
$22.00
Add to cart
Rated 4.00 out of 5